Children get hospitalized for depression and bipolar disorders.
I wasn’t aware of how frequently this happens until I got my hands on some BIG DATA – the HCUP KID database of children’s hospitalizations. My colleagues and I analyzed hospitalizations in 2000, 2003 and 2006 and published our results in the journal, Child and Adolescent Psychiatry and Mental Health in 2011. For each of these years, we were able to look at records for over 2 million hospitalizations, and able to project these to the entire number of pediatric hospitalizations in the US in those years.
Some take home points
Percentages of hospitalizations where the principal diagnosis was a mental health diagnosis
- In children age 15-17, 13.7 to 15.2% of hospitalizations had a mental health principal diagnosis
- In children age 10-14, 15.0 to 15.6% of hospitalizations had a mental health principal diagnosis
- In children age 5-9, 4.4 to 4.8% of hospitalizations had a mental health principal diagnosis accounted
The incidence of hospitalizations with mood disorders as the principal diagnosis compared to the entire population of children
12.1-13.0 out of every 10,000 children were hospitalized with mood disorders as the principal diagnosis in 2000-2006.
Age
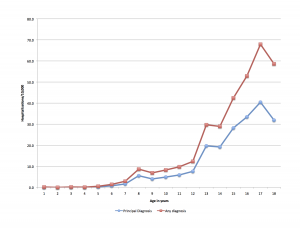
The incidence of hospitalizations for children with mood disorders increased with age – this figure uses data from 2006 to show the trend.
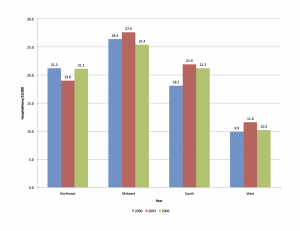
Region of the country
A surprising finding was the big differences between regions of the country. As an example, in 2006, the Western region experienced the lowest rates (10.2/10,000) while the Midwest had the highest rates (25.4/10,000). This figure shows the rates for 2000, 2003 and 2006.
Did you know?
Mood disorders including depression and bipolar disorders are a major cause of morbidity in childhood and adolescence, and hospitalizations for mood disorders are the leading diagnosis for all hospitalizations in general hospitals for children age 13 to 17.
Between 2000 and 2006, inflation-adjusted hospital charges increased from $10,600 to $16,300.