What are pharmacy deserts?
You’ve heard the term “food deserts” – defined by USDA as, “urban neighborhoods and rural towns without ready access to fresh, healthy, and affordable food”. Pharmacy or medication deserts are analogous. The researchers who coined the phrase note they are defined by
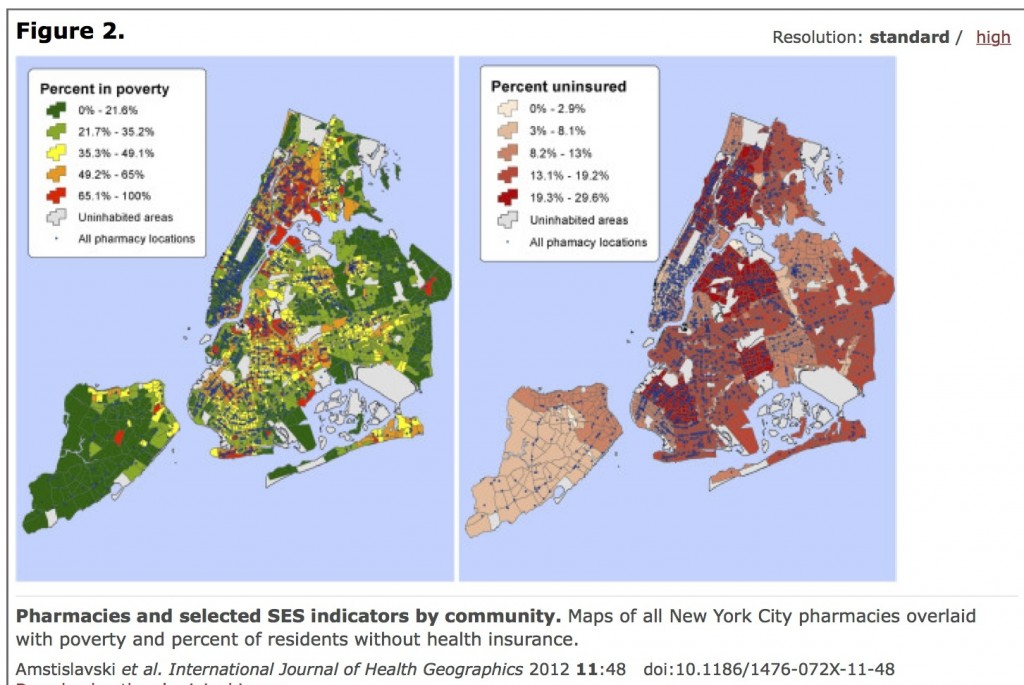
“the low availability of the most commonly dispensed prescription medications in these areas.” (Amstislavski et al, 2012).
The concept builds on earlier geographic work examining not only the location of pharmacies, but variations in how pharmacies are stocked in neighborhoods of lower socio-economic status, or neighborhoods with large African-American or Hispanic populations. Researchers (and pharmacy student research assistants) mapped pharmacies in neighborhoods throughout New York City, and obtained information about pricing and stock availability for 13 frequently prescribed medications. They found variability in pricing as well as the pharmacy’s stocking of the prescriptions, and concluded,
“In extreme cases, entire communities could be deemed ‘medication deserts’ because geographic access to pharmacies and the availability of the most prescribed medications within them were very poor.”
Awareness of the role of pharmacies in access to care is growing.
The journal, Health Affairs, just published an article on Pharmacy Deserts in Chicago, “‘Pharmacy Deserts’ Are Prevalent In Chicago’s Predominantly Minority Communities, Raising Medication Access Concerns” (Qato et al, 2014), and the National Community Pharmacists Association (NCPA) picked up on this issue in a commendable way, noting that,
“About 32 percent of Chicago’s 802 communities were “pharmacy deserts,” meaning their residents met the researchers’ criteria for both low pharmacy access and low income.”
They also noted that,
“Between 2000 and 2012, pharmacy disparities worsened. While the number of pharmacies (particularly chains) in majority-white communities increased 20 percent during that time period, there was no such expansion in minority communities.”
These recent studies underscore the importance of taking a broad approach when considering access to care and treatments. Patients with insurance coverage may have limited access to care if they live in neighborhoods without pharmacies, or if the pharmacies in their neighborhood don’t stock needed medications.
If you’re interested in the issue of access to pharmacies take a look at these earlier publications:
- Bernstein et al., Disparities in access to over-the-counter nicotine replacement products in New York City pharmacies. Am J Public Health. 2009 Sep;99(9):1699-704.
- Cooper H, Bossak B, Tempalski B, Friedman S, Des Jariais D. Temporal trends in spatial access to pharmacies that sell over-the-counter syringes in New York City health districts: relationship to local racial/ethnic composition and need. J Urban Health. 2009;86(6):929-945.
- Morrison RS, Wallenstein S, Natale DK, Senzel RS, Huang LL. “We don’t carry that”–failure of pharmacies in predominantly nonwhite neighborhoods to stock opioid analgesics. N Engl J Med. 2000;342(14):1023-1026.