“What Pharmacists Need to Know About Racial and Ethnic Health Disparities”, available on iBooks
iBooks lets you browse books and download them directly to your Mac®, iPad®, iPhone®, or iPod® touch.
The same content as the print book with the added convenience of
- Interactive Images with callouts, pan-and-zoom, and pop-overs.
- Scrolling Sidebars to cover relevant asides and tangential topics.
- Highlighting and study cards – Use your finger as a highlighter when you’re reading a book on your iOS device or Mac. Just swipe over the selected text (using the trackpad on your Mac), and it’s highlighted. Notes and highlights automatically appear on study cards.
- iBooks supports updates – that means if a book you purchased is republished with new or additional content, iBooks lets you know. You can download the updated version free, and it automatically replaces the older copy in your library.
A text for use in public health, health disparities, health services research, and related courses
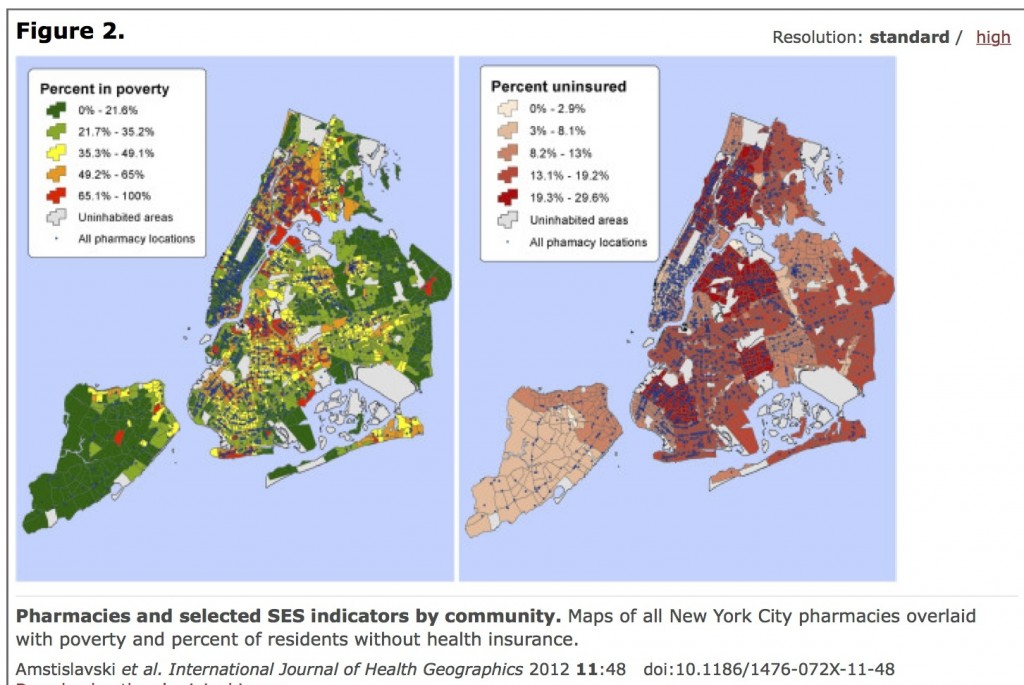
for pharmacy students in their second, third, and fourth years of training. Discusses the concepts of race and ethnicity and the constructs used to classify and categorize them and provides an overview of the data collected regarding disparities in mortality, morbidity, provision of health care, and other health indicators and epidemiologic studies of mechanisms and pathways. Addresses racial and ethnic health disparities that can occur in real-world pharmacy care, such as differences in disease conditions, response to medication, access to care, health literacy, and understanding of health and medications.
As reviewed in the American Journal of Pharmaceutical Education